Your Wellbeing Starts Here.
Welcome to Lakeland Care!
We are so glad you are here.
At Lakeland Care, Inc. (LCI), our heart and soul is linked to Empowering Individuals. Strengthening Communities. Inspiring Futures. This is fulfilled in supporting those we serve and the communities we touch. For more than two decades we have worked tirelessly to redefine health and wellness for some of Wisconsin’s most at-risk populations. As a private, non-profit, organization, Lakeland Care delivers a unique approach to managed care with person-centered services through a variety of programs. Our goal is to help those we serve to live as independently as possible because we know how important it is to remain connected to family, friends, and community.
We believe in you.
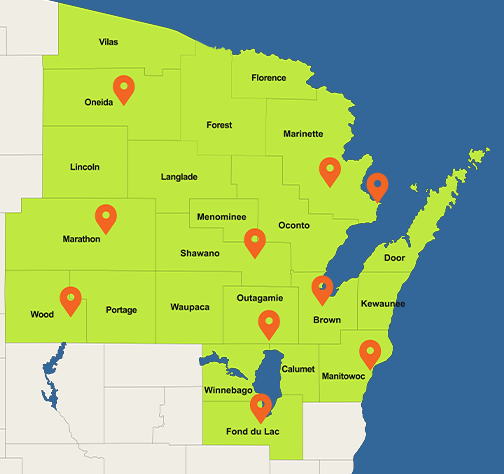
Lakeland Care offers the Family Care program under a contract with the Wisconsin Department of Health Services/Medicaid and was one of the first Managed Care Organizations to provide the Family Care benefit in the state more than 20 years ago. Family Care helps eligible elders and adults with disabilities live independently at home and in their community. Lakeland Care is a proud steward of Medicaid dollars, through partnership with over 1,000 local providers. We spend 96% of every Medicaid dollar directly supporting care for members across 22 counties and two Tribes in Northeast and North Central Wisconsin. We look forward to including you in our Lakeland Care family where together, we build better lives.
And we aren’t slowing down.
Lakeland Care is diversifying its business in innovative ways to create a world we all want to live in. Lakeland Care now offers several consulting program and service options to support community businesses and individuals. These offerings work to enhance leadership skills, advance organizational effectiveness, and workplace cultural excellence. Lakeland Care has also launched a private care management program, Care Plus, which is designed to coordinate care and services needed for individuals to live their happiest, healthiest, most independent life. These new programs address the needs of our communities and the individuals within them, empowering individuals, strengthening communities, and inspiring futures.
Meet Our Members